Parkinson’s Beyond the Brain


By Emma Yasinski
BU News Service
By the time a patient is diagnosed with Parkinson’s disease, seventy percent of the damage is already done. In an effort to understand the progression of the disease and diagnose it earlier, more and more scientists are moving their microscopes to the patient’s gut.
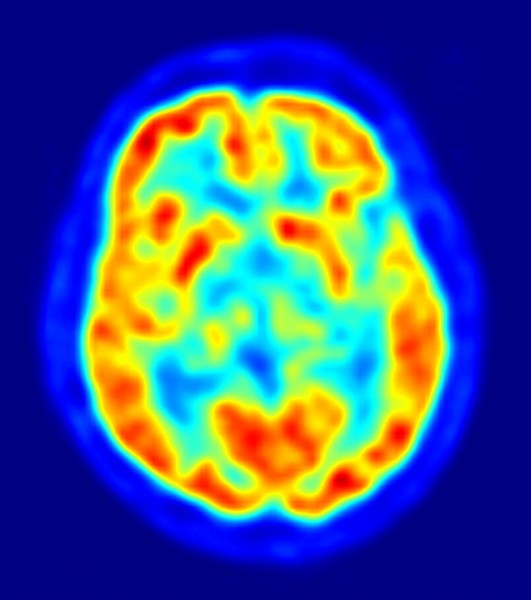
Researchers agree that the most characteristic traits of Parkinson’s disease, difficulties with movement, are caused by protein clumps found in the substantia nigra, a small area deep in the brain. In 2003, renowned researcher, Heiko Braak, PhD at Johann Wolfgang Goethe University in Germany, proposed a theory that rather than starting in the brain, the disease might start elsewhere in the body. Based on patterns he observed in autopsies, he proposed that alpha-synuclein, the protein considered to be the main cause of damage in the Parkinson’s brain, might spread from nerve cell to nerve cell. He suggested the protein might start outside the brain and travel through nerve cells up to the substantia nigra. Before this, most researchers believed that these proteins aggregated only in the substantia nigra- and nowhere else. His proposal completely changed the way researchers thought about the progression of the disease.
Dr. Kathleen Shannon of Rush University Medical Center in Chicago was in the middle of reading Braak’s 2003 study when she received an email from her new collaborator, a gastroenterologist. He was at a conference in another state, learning about Parkinson’s because a family member had been recently diagnosed with the disease. He perked up when he heard researchers describe a new rodent model for the disease. The model used a neurotoxin called lipopolysaccharide to induce symptoms. As a gastroenterologist, he recognized the toxin. “Did you know the only route of exposure is through the intestinal system?” His email to Shannon stated that this was their next clue to a new understanding of the disease. If this toxin is entering through the intestines and leading to Parkinson’s-like symptoms, maybe the real disease pathology works this way too.
They immediately recruited nine patients who were recently diagnosed with Parkinson’s, but had not yet begun treatment. The first goal was to test whether the patients had a “leaky gut” – a condition in which pathogens are able to move across the intestinal wall more easily than usual. They gave the patients several different types of sugars and then tested for their presence in the patients’ urine. Depending on the ratio of different sized sugars found in the urine, the researchers were able to tell how permeable, or “leaky” each patient’s colon was. Those that had been recently diagnosed with Parkinson’s showed evidence of significantly leakier guts than healthy patients.The patients’ intestines also showed evidence of alpha-synuclein, the protein most closely associated with Parkinson’s disease. The researchers hypothesized that the body might start producing protein in response to a toxin that enters through the leaky intestinal walls.
The following year the researchers tracked down biopsies from three of their patients’ past colonoscopies. The researchers’ goal was to see if alpha-synuclein was present in the intestines prior to the onset of Parkinson’s symptoms. The samples came from 2-5 years before the individuals were diagnosed with Parkinson’s. All three patients’ biopsies showed alpha-synuclein in the colon. In contrast, she found no evidence of alpha-synuclein in the colons of the 23 healthy patients. This was the first study showing that the protein could be found in the gut prior to a patient’s diagnosis.
Several teams of researchers are currently working to validate this finding with larger sample sizes. If they find the same results, doctors could diagnose Parkinson’s disease earlier than ever, during a routine colonoscopy. Earlier diagnosis of the disease would make it possible to begin treatment earlier before most of the neurons are already damaged. Right now, doctors can only diagnose the disease when the patient displays motor symptoms. By then, 70% of the neurons in the substantia nigra are dead. It’s possible that an ability to diagnose the disease earlier would allow researchers to intervene, and maybe even find a way to slow or prevent the cell death.
Early diagnosis is only one benefit to elucidating the roots of alpha-synuclein in the body. As researchers gain a better understanding of Parkinson’s, Shannon hopes they can work backwards to create better animal models. She explained that current animal models only mimic the disease’s effects on the brain, and not the rest of the body. Researchers create one of the most common models by damaging the neurons in the substantia nigra of rats’ brains. If scientists hope to develop treatments that target pathology or symptoms outside of the brain, they will need more accurate models, which mimic the disease pathology throughout the body. Beth Vernaleo, PhD., Senior Manager of Research Programs at the Parkinson’s Disease Foundation, described a lack of accurate animal models as one of the greatest challenges facing Parkinson’s researchers. “You have to start there.” She said “When you’re looking at things like colonoscopy samples, you’re hypothesizing what’s happened. You have to look back at biological models to see if it’s actually what is happening.”
Some researchers still aren’t convinced. Thomas Beach, PhD, Director of the Brain and Body Donation Program at Banner Sun Health Research Institute, does not believe that Parkinson’s disease pathology starts outside of the brain at all. His research, based on an extensive collection of autopsies, suggests that while the patient may not have symptoms until the pathology has reached other areas of the body, it still begins in the brain, “We have never detected alpha-synuclein deposits in the body unless they were already somewhere in the brain,” he said “It does not start in the body. It starts in the brain and moves to the body after.” He does, however, agree that the alpha synuclein deposits throughout the body could be useful for confirming diagnosis and treating specific symptoms of the illness.
Whether scientists hope to find a diagnostic marker, a treatment, or an animal model, it seems most researchers and patients agree that looking to the intestines is an important new step in Parkinson’s disease research. And the trend is catching on. Researchers specializing in other neurological diseases, such as Multiple Sclerosis and Alzheimer’s disease, are following suit and looking at changes in the gut to understand the illnesses. A group of researchers at several different institutions across the United States has come together to create the Multiple Sclerosis Microbiome Consortium (MSMC) to share information on the topic. Charlotte Madore, PhD at Brigham and Women’s Hospital, has just started a study about the relationship between the gut microbiota and cells that lead to inflammation in the brain. If there is a relationship between the two, it will be a crucial piece of the puzzle not just in Parkinson’s, but all neurodegenerative diseases.
As of right now, doctors have no way to stop the progression of these diseases; all they can do is temporarily alleviate the symptoms. Perhaps the keys to reversing them lie in the gut.